Umbilical Cord Blood in Rare Disease Treatment
Umbilical cord blood, once discarded after childbirth, is now a critical tool for treating rare genetic disorders. Its unique stem cells can regenerate blood and immune systems, offering hope for conditions like sickle cell disease, Krabbe disease, and Hunter syndrome. Unlike bone marrow, cord blood doesn’t need a perfect donor match, making it accessible for diverse populations. Research shows it can halt disease progression, improve survival rates, and even reverse some symptoms when used early. With storage lasting decades, cord blood banking ensures families have immediate access to life-saving treatments for over 80 FDA-approved conditions and emerging therapies for future needs.
Recent Study Results
Cord Blood Treatment Success Rates for Rare Genetic Disorders
UPMC Children's Hospital Study on Genetic Disorders
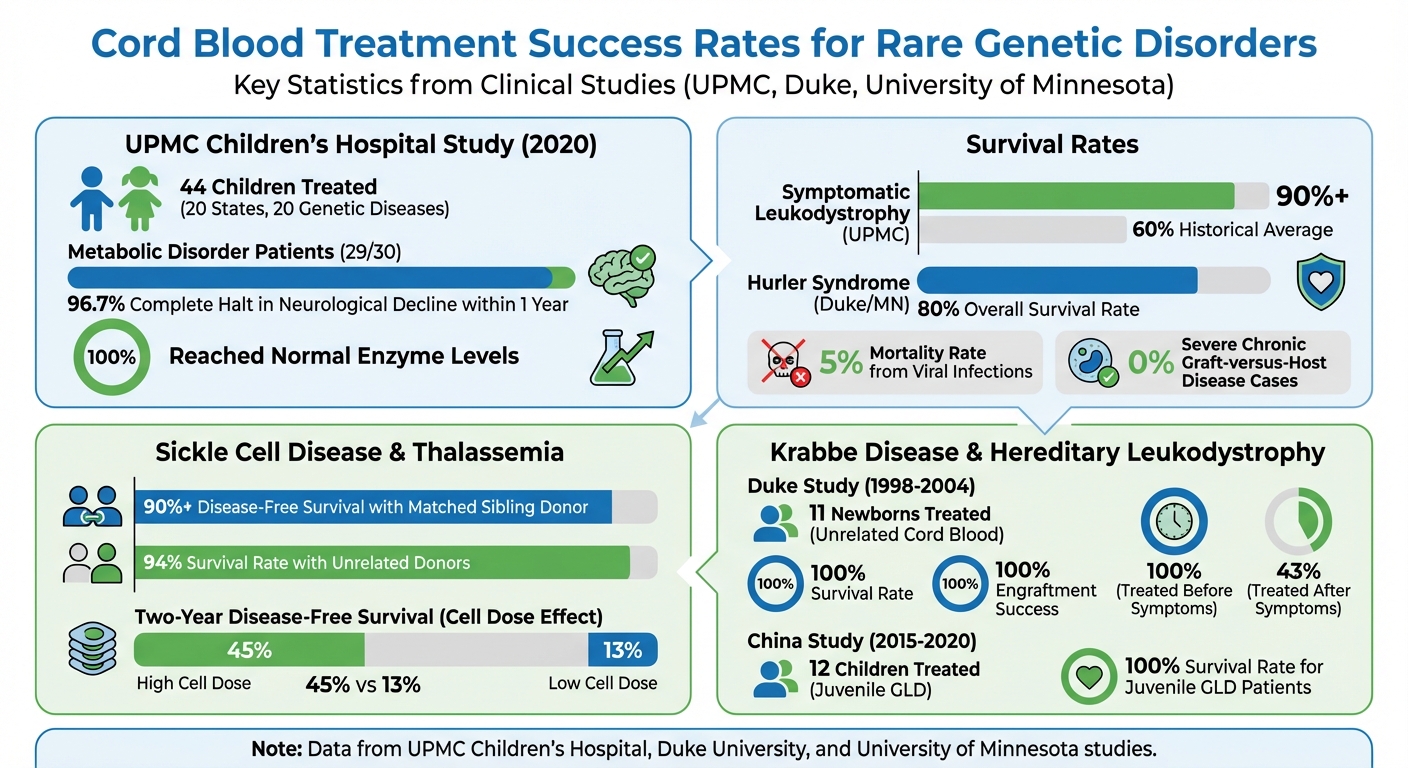
In July 2020, UPMC Children's Hospital of Pittsburgh shared groundbreaking results in Blood Advances. Dr. Paul Szabolcs led the study, which included 44 children from 20 states and addressed 20 different genetic diseases such as sickle cell, thalassemia, Hunter syndrome, Krabbe disease, and metachromatic leukodystrophy.
The team introduced a "universal" treatment strategy. Instead of crafting separate therapies for each rare condition, they employed a Reduced-Intensity Conditioning (RIC) regimen - a carefully balanced mix of low-dose chemotherapy and immunotherapy. This method aimed to protect critical organs like the heart, lungs, and kidneys while ensuring the transplant wasn't rejected.
One standout innovation was the "plug-in" immune boost technique. A small portion of the original cord blood was frozen and later reinfused one to two months after the transplant. This approach accelerated immune recovery, helping patients rebuild their defenses more quickly. Among the 30 children with metabolic disorders, 29 experienced a complete halt in neurological decline within a year. All reached normal enzyme levels, and some even began regaining skills they had lost.
"We designed an approach now proven efficacious for at least 20 diseases."
Safety and Success Rates of Cord Blood Infusions
The treatment's safety outcomes were just as encouraging as its effectiveness. For symptomatic leukodystrophy patients using the UPMC protocol, the three-year survival rate topped 90%, a significant improvement over the historical average of 60%. The mortality rate from viral infections due to immune suppression was only 5%, and there were no cases of severe chronic graft-versus-host disease - a common and serious transplant complication.
A separate long-term study of 25 Hurler syndrome patients, conducted by Duke University and the University of Minnesota, reported an 80% overall survival rate. These patients achieved full donor chimerism (over 90% donor cells), maintained normal enzyme levels, and showed developmental progress, including normalized head circumference and reduced brain atrophy. Together, these findings highlight the potential of cord blood therapies in treating rare genetic disorders effectively and safely.
sbb-itb-df90ce4
Rare Diseases Treated with Umbilical Cord Blood
Clinical studies have shown how umbilical cord blood can play a game-changing role in treating various rare diseases.
Sickle Cell Disease and Thalassemia
Umbilical cord blood transplants have shown impressive results in addressing these inherited blood disorders. For patients with a matched sibling donor, the success rate is striking, with over 90% achieving disease-free survival. The procedure works by replacing the bone marrow that produces defective red blood cells with healthy stem cells derived from cord blood.
The total cell dose is a critical factor for success. For instance, patients receiving grafts with more than 5 × 10⁷ total nucleated cells per kilogram experienced a two-year disease-free survival rate of 45%, compared to just 13% for those with lower doses. In cases where unrelated donors were used for sickle cell disease, survival rates reached 94%. However, disease-free survival dropped to 50%, largely due to higher rates of graft rejection. With around 7% of the global population carrying a hemoglobinopathy mutation and only 14% of sickle cell patients having access to a matched sibling donor, cord blood offers a vital alternative.
These results open the door for exploring cord blood's potential in treating other genetic conditions.
Hunter Syndrome and Krabbe Disease
Cord blood transplants have proven effective for lysosomal storage disorders like Hunter syndrome and Krabbe disease by delivering enzymes directly to the brain - something conventional enzyme therapies struggle to achieve. Between 1998 and 2004, Duke University Medical Center treated 11 newborns with infantile Krabbe disease using unrelated cord blood. The results were remarkable: all 11 patients survived, with a median follow-up of three years, achieving 100% engraftment and normal enzyme levels in their blood.
Timing is crucial. Infants treated before symptoms emerged had a 100% survival rate, while those who began treatment after symptoms appeared saw their survival rate drop to 43%.
Leukodystrophies and New Treatment Approaches
Cord blood is also being used to tackle neurological disorders, offering hope for conditions like leukodystrophies, where nerve fibers lose their protective myelin coating. The donor cells from cord blood transform into microglia in the brain, delivering enzymes that help maintain myelin and slow neurological decline.
Since 1981, over 2,500 patients with inherited metabolic diseases have undergone transplants. Cord blood is increasingly favored over bone marrow, especially for rapidly progressing conditions, as it provides higher long-term enzyme levels. For example, patients with Hurler syndrome treated with cord blood achieved significantly better enzyme levels after nine years than those treated with bone marrow. Another advantage is that cord blood transplants allow for more flexibility in HLA matching, working effectively with 4/6 or 5/6 matches. This is particularly beneficial for ethnic minority patients, who often face challenges finding perfect matches in adult donor registries.
Current Research in Rare Disease Treatment
Researchers are actively investigating new ways to use cord blood to treat rare genetic disorders, with promising developments in several areas.
Neuronal Ceroid Lipofuscinoses (NCLs)
Early findings suggest that cord blood transplants could offer benefits for patients with Neuronal Ceroid Lipofuscinoses (NCLs), a group of conditions that includes Batten disease. Although still in its infancy, this research has shown encouraging short-term results in pilot studies. Scientists are focusing on the role of specific proteins, such as those associated with the CLN8 gene, which are critical for cell growth and protection against cell death. Understanding these mechanisms could pave the way for more precise treatments, such as cellular or gene-based therapies.
Cord blood is also making strides in the treatment of inherited metabolic disorders, building on its success in other genetic conditions.
Inherited Metabolic Disorders
In the realm of inherited metabolic disorders (IMDs), cord blood has become a preferred treatment at many specialized centers. Recent research has addressed the challenge of delayed donor cell engraftment, achieving survival rates of over 95% for successful engraftment. For instance, between April 2015 and March 2020, the Children's Hospital of Fudan University in China treated 12 children with hereditary leukodystrophy using unrelated cord blood transplants. Led by Xiaowen Qian and Xiaowen Zhai, the study reported a 100% survival rate among juvenile globoid cell leukodystrophy (GLD) patients, along with stable neurological function scores post-transplant.
To address the months-long delay before donor cells fully populate the brain with enzyme-producing microglia, researchers are exploring adjuvant cell therapies. One such approach involves DUOC-01, a therapy using oligodendrocyte-like cells derived from the same cord blood unit as the transplant. These cells are delivered via intrathecal injection to provide early enzyme replacement in the brain. A clinical trial (NCT02254863) conducted from 2015 to 2017 tested this method, showing promise for rapidly progressing diseases where even small timeframes are critical.
What This Means for Families
How Cord Blood Banking Supports Rare Disease Treatments
Recent advancements highlight how banking cord blood can provide families with crucial options when faced with urgent medical needs. For those dealing with rare genetic disorders, cord blood banking ensures quick and dependable access to life-saving stem cells. In cases like Krabbe disease or Hurler syndrome, having cord blood stored eliminates the often lengthy process of finding a compatible donor - a delay that could be critical for fast-progressing conditions.
One of the biggest advantages is the perfect match it offers. Banked cord blood is a 100% match for the child and often matches siblings or other family members, reducing the risks of transplant rejection. Americord Registry uses advanced storage techniques, such as 5-compartment vials, allowing a single collection to support multiple treatments. Additionally, their quality guarantee ensures treatment options remain viable even if the sample fails to engraft.
Families with a history of genetic conditions benefit greatly when cord blood is collected at birth, especially if transplantation occurs before symptoms develop. Early treatment with banked cord blood has shown significantly better survival rates and developmental outcomes compared to untreated cases, making preparation a vital step.
Future Treatment Possibilities
The potential uses for cord blood are expanding well beyond the 80+ FDA-approved treatments currently available. Ongoing research includes over 300 clinical trials worldwide, exploring its application for conditions like autism, cerebral palsy, and various metabolic disorders. Dr. Paul Szabolcs’s UPMC protocol has already been successfully applied to more than 20 diseases, with hopes it could address many more in the future.
Families now have the option to store not just cord blood but also cord tissue and placental tissue, which contain mesenchymal stem cells (MSCs). These cells are being studied for their potential in regenerative therapies, including organ, muscle, and bone repair. With cryopreservation keeping stem cells viable for decades - up to 200 years - this offers a long-term safety net for medical needs. These advances highlight cord blood’s growing role in personalized medicine and forward-thinking treatment options.
Conclusion
Umbilical cord blood has emerged as a proven treatment option for rare genetic disorders, supported by recent research and advancements. The protocol developed at UPMC Children's Hospital has delivered impressive results across various conditions. As Dr. Paul Szabolcs put it:
"The regimen we developed is more robust, readily applicable and will remain significantly less expensive" than creating individual gene therapies for each rare disease.
For families navigating these challenges, timing is everything. Banking cord blood at birth eliminates the need for a prolonged search for compatible donors and allows treatment to begin before irreversible damage sets in. This proactive step can be life-changing.
These breakthroughs also reduce treatment delays and ensure donor availability when it matters most. Americord Registry expands on this progress by offering preservation services that go beyond cord blood, including cord tissue and placental tissue. This approach increases the variety of stem cells available, broadening potential treatment options for both current and future medical needs. With hundreds of clinical trials underway and stem cells remaining viable for decades through cryopreservation, families gain a long-term safeguard for conditions that may not yet have a cure.
Cord blood banking is transforming how rare diseases are treated. By preserving these cells at birth, parents open the door to life-saving treatments today and untapped possibilities for the future.
FAQs
What makes umbilical cord blood treatment different from bone marrow transplants?
Umbilical cord blood and bone marrow transplants both rely on stem cells, but the way these cells are sourced and used sets them apart. Cord blood is collected immediately after birth from the umbilical cord and placenta. This process is completely non-invasive and uses what would otherwise be discarded. On the other hand, bone marrow transplants involve extracting stem cells directly from a donor’s bone marrow, which is a more invasive and complex procedure.
Cord blood transplants have shown promise in addressing rare genetic conditions like Krabbe disease and cerebral palsy. They also tend to cause fewer complications, such as graft-versus-host disease, making them particularly effective for children. Another advantage is that cord blood can be stored for future use, offering a practical option for advancing regenerative medicine.
What are the benefits of storing umbilical cord blood for future medical treatments?
Storing umbilical cord blood offers a one-of-a-kind chance to preserve stem cells, which play a critical role in treating over 80 diseases. These include leukemia, lymphoma, and various immune and blood disorders. Stem cells from cord blood are particularly versatile and carry a lower risk of complications like graft-versus-host disease during transplants, making them an important tool in regenerative medicine.
Emerging research also points to the promise of cord blood in addressing rare genetic conditions like sickle cell disease, Krabbe disease, and Hunter syndrome. By choosing to bank cord blood at birth, families can secure a potential lifeline that may broaden treatment possibilities and improve future health outcomes for loved ones.
How effective is umbilical cord blood in treating rare genetic conditions like Hunter syndrome and Krabbe disease?
Umbilical cord blood has been making waves in the treatment of rare genetic conditions like Hunter syndrome and Krabbe disease. Clinical studies have demonstrated its effectiveness and safety when used in therapies involving infusions from healthy donors.
What makes cord blood stem cells so special? They have unique regenerative properties that aid in repairing and restoring function in affected patients. While research continues to push boundaries, the results so far highlight the promise cord blood holds in tackling these challenging genetic disorders.
The views, statements, and pricing expressed are deemed reliable as of the published date. Articles may not reflect current pricing, offerings, or recent innovations.